Group B streptococcal (GBS) infection remains the most common cause of neonatal early-onset sepsis and a significant cause of late-onset sepsis among young infants. Administration of intrapartum antibiotic prophylaxis is the only currently available effective strategy for the prevention of perinatal GBS early-onset disease, and there is no effective approach for the prevention of late-onset disease.
The American Academy of Pediatrics joins with the American College of Obstetricians and Gynecologists to reaffirm the use of universal antenatal microbiologic-based testing for the detection of maternal GBS colonization to facilitate appropriate administration of intrapartum antibiotic prophylaxis.
The purpose of this clinical report is to provide neonatal clinicians with updated information regarding the epidemiology of GBS disease as well current recommendations for the evaluation of newborn infants at risk for GBS disease and for treatment of those with confirmed GBS infection.

History
The Centers for Disease Control and Prevention (CDC) first published consensus guidelines on the prevention of perinatal group B streptococcal (GBS) disease in 1996.
These guidelines were developed in collaboration with the American Academy of Pediatrics (AAP), the American College of Obstetricians and Gynecologists (ACOG), the American College of Nurse-Midwives, the American Academy of Family Physicians, and other stakeholder organizations1 on the basis of available evidence as well as expert opinion.
The 1996 consensus guidelines recommended an antenatal either culture–based or risk factor–based approach for the administration of intrapartum antibiotic prophylaxis (IAP) to prevent invasive neonatal GBS early-onset disease (EOD). The guidelines were updated in 2002 and 2010.
Evolving epidemiology, newly published data, and changing practice standards inform periodic review of practice guidelines. In 2017, representatives from the CDC, AAP, ACOG, and other stakeholder organizations agreed to review and revise the 2010 GBS guidelines.
Early-Onset-Diseases GBS Infection
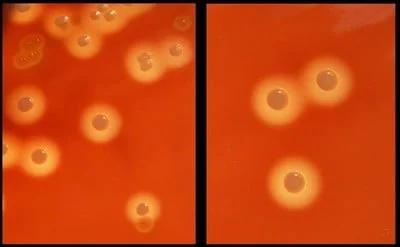
GBS EOD defined as isolation of group B Streptococcus organisms from blood, cerebrospinal fluid (CSF), or another normally sterile site from birth through 6 days of age.
Observations have shown that, most often, early GBS infection has developed in such categories of babies:
- premature (<37 weeks) - 28% of all cases of the disease;
- birth weight less than 1500 g - approximately 15% of cases of early GBS.
The greatest danger is meningitis, which noted in 9.5% of infection episodes.
The risk of death in early GBS infection is higher in premature babies (19.2% of cases) than in newborns with normal body weight (2.1% die).
Signs of an acute infection process usually develop during the first 48 hours after birth.
Late-Onset GBS Disease
Exhibited when detecting SGB in normally sterile tissues of an infant 7-89 days old. The average age of sick babies is 34 days (20-49 days).
Infections after 3 months of life are sporadic and inherent in children with deep prematurity or immunodeficiency states. Among the patients, more than 42% were newborns weighing less than 1500 g. As with early infection, the development of meningitis is the greatest danger.
Interestingly, the introduction of intrapartum antibiotic prophylaxis had little effect on the incidence of GBS infection in the late period.
Pathogenesis and risk factors
An obligatory factor in terms of the risk of developing an early GBS in an infant is contamination of the mother's genital tract by this pathogen. The child becomes infected either in the early patrimonial period, by swallowing infected amniotic fluid, or by seeding the oral cavity and intestinal tract during birth through the birth canal.
With respect to premature babies, a reverse mechanism is possible: intraamniotic infection leads to too early childbirth. In addition, the fetus becomes infected with GBS shortly before delivery.
The risk is big enough. So, in the USA, colonization of the genital tract by streptococci of group B noted in 20-30% of pregnant women.
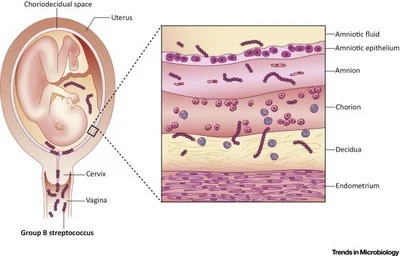
Without the appointment of intrapartum antibiotic prophylaxis, GBS infects more than 50% of newborns. An acute infectious process develops in 1-2% of babies.
Chance to get sick more in the presence of such risk factors:
- prematurity of the fetus due to the immaturity of the immune systems;
- early rupture of amniotic fluid and rupture of amniotic membranes;
- mother-to-fetus fever;
- development of GBS infection in the previous child (if the mother’s birth is repeated).
There are researchers who see unqualified gynecological and obstetric manipulations as a risk of infection of the fetus with streptococci. But there is no serious evidence that they are right.
As for the late GBS infection, the microbiome of the genital tract of the mother does not play an important role. More significant is the relationship with infant infection as a result of communication with other people. This thesis confirmed by the high incidence of late UBC infections in premature (less than 37 weeks) infants with immature immune mechanisms.
Prevention of perinatal GBS infection
Numerous observational and one randomized controlled trial confirm the prophylactic efficacy of antenatal maternal antibiotics. It is believed that the interruption of the vertical transmission of infection is implemented by the following mechanisms:
- Reducing the number and activity of streptococcus microbiome of the mother.
- Prevention of colonization of the mucous membranes of the fetus / newborn.
- Formation in the blood of the fetus / infant of therapeutic concentrations of antibiotic that prevent the development of GBS infection.
In order to identify indications for prescribing a prophylactic course, it recommended to conduct bacteriological examination of vaginal-rectal cultures for all pregnant women in the period 36-37 weeks.
An alternative is the nucleic acid amplification test with GBS smears, urine. Such screening should be carried out in women with the prospect of imminent labor.
An indication for the purpose of a preventive course is a positive result of any study.

Antibiotic prophylaxis is prescribed to unexamined women and those whose results were negative in the event of such events:
- The body temperature in giving birth mother 38 degrees and above.
- Since the rupture of the membranes more than 18 hours have passed.
- In previous births, the fact of the GSS carriage was established.
Preparations for the prevention
It is necessary to adhere to drugs of low toxicity and high activity. Current recommendations offer:
- Ampicillin. 97% reduced contamination of the genital tract of the mother within 2 hours after administration. Penetrates through the placenta and "covers" the child.
- Penicillin. The effects are the same, the spectrum is narrower, which makes the drug more preferable than ampicillin.
- Cefazolin. When allergic to lactam antibiotics. Penetrates through the placenta. Therapeutic concentration in cord blood and amniotic waters within 20 minutes after the introduction of the mother.
- Clindamycin. When allergic to penicillins and confirmed sensitivity of streptococci to clindamycin (42% of isolates resistant).
- Vancomycin. If you are allergic to penicillins and microorganism resistance to clindamycin. Therapeutic concentrations in cord blood are reached after 30 minutes.
Dosage selected based on body weight of the mother. Antibiotics themselves have no negative effect on the fetus.
Findings
The widespread introduction of screening for GBS, an objective assessment of the risk of developing an infection, helps to reduce the likelihood of an acute infection process in an infant.
In the following publication, we will look at the recommendations of the American Academy of Pediatrics for the treatment of newborns with an infection caused by group B streptococcus.