Exercise-induced purpura, which has also been called “golfer’s purpura,” is a phenomenon that has been rarely reported in the pediatric literature. This is the first case series in which this benign vasculopathy, which is most often associated with warm weather and high-impact activity, is described. In this series, we describe 5 patients, most of whom had an erythematous purpuric rash above the sock line that extended to the knees and was associated with warm weather and prolonged activity. Exercise-induced purpura may be mistaken for Henoch-Schönlein purpura or as a manifestation of a possible systemic vasculitis. Recognition of this benign condition is vital to avoid an unnecessary workup and a costly evaluation with accompanying anxiety.
Abbreviations:
- EIP — exercise-induced purpura
- LCV — leukocytoclastic vasculitis
Exercise-induced purpura (EIP), which has also been called “golfer’s purpura,” has been described in the adult literature but rarely in the pediatric population. EIP typically appears as a petechial rash and occurs in warm weather after prolonged, weight-bearing activity. It is predominantly localized symmetrically to the lower extremities and typically appears above areas of compression, such as socks. To date, there has only been 1 case of this benign vasculopathy reported, which presented atypically. In this case series, we describe 5 patients with EIP who presented between the ages of 8 and 15 years.
Case Descriptions
Case 1
Patient 1 was a white boy who presented at the age of 8 years with an episodic petechial rash extending from his ankles to the knees that occurred twice per month for 3 months and lasted for 2 to 3 days at a time. A diagnostic workup revealed a normal complete blood count and erythrocyte sedimentation rate and normal C-reactive protein, creatinine, and urine protein and/or creatinine levels. He was initially diagnosed with suspected Henoch-Schönlein purpura by the pediatric rheumatologist.
Over the next 2 years, he had recurrent episodes of the rash preceded by sun exposure and high-impact activity. Further laboratory investigations were performed, with normal results (see Table 1). On the basis of the history and negative diagnostic workup, he was diagnosed with EIP. No therapy was initiated.

Case 2
Patient 2 was a Hispanic girl who presented at the age of 8 years with a petechial rash appearing above her sock line and extending to her upper shins. The rash only appeared during warm weather and after prolonged physical activity, including hiking and a 4-day field hockey camp. The rash typically lasted between 2 and 7 days. On the basis of the location of the rash and the history of it occurring in the heat with prolonged activity, a diagnosis of EIP was made. No further diagnostic workup was completed. Naproxen was prescribed but did not help to resolve the rash and was subsequently discontinued.
Case 3
Patient 3 was an Asian American girl who presented at the age of 15 years with bilateral ankle and knee pain as well as a nonpruritic, nonpainful petechial rash localized to her bilateral shins. The rash was described to be recurrent during the summer, primarily with high-impact activity and particularly when she was dancing, up to 5 times per week. The rash lasted ∼1 week per occurrence. Results of her laboratory evaluation were normal except for a urinalysis with trace hemoglobin, which resolved on repeat testing (see Table 1). On the basis of her history and a normal workup, the diagnosis of EIP was made. Topical triamcinolone was trialed for the rash but was discontinued on the basis of the patient reporting pruritis with use of the cream.
Case 4
Patient 4 was a white girl who presented at the age of 12 years with an intermittent rash for 5 years. The rash appeared as nonpruritic, nonblanching, and nonpalpable erythematous petechiae that extended from her ankles up to her thighs and occasionally on her arms, with the most prominent lesions being just above the sock line.
The rash would last for 3 to 4 days, and the preceding trigger was high-impact activity, including participation in field hockey and lacrosse. The duration of the physical activities was directly related to the intensity of the color and the duration of the rash.
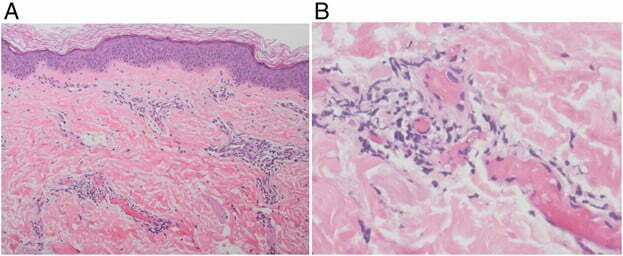
Results of laboratory evaluations were normal (see Table 1). A skin biopsy was performed and revealed a perivascular neutrophilic infiltrate with nuclear debris, with hemorrhage and few erythrocyte extravasations most consistent with leukocytoclastic vasculitis (LCV). On the basis of the history of rash occurrence during sports in the warm weather and a normal diagnostic workup, a diagnosis of EIP was made. She was given colchicine as a treatment option, which did not lessen the frequency of episodes and was therefore discontinued.
Case 5
Patient 5 was a white boy who presented at the age of 15 years with an intermittent petechial rash above the sock line extending to the mid-anterior shin that appeared after working in a corn maze during the summer. He reported that his rash normally lasted 4 days. He did not have the rash in cold weather or if he worked for a short period. Results of laboratory evaluations were normal (see Table 1). On the basis of his presentation, the diagnosis of EIP was made. No treatment was initiated.
Discussion
EIP is a benign vasculopathy that can occur in children or adults. This is the first case series in which this entity is described in children. Recognition of the appearance and typical presentation can prevent anxiety and concern by patients and parents as well as an unnecessary and costly workup. The patients in this case series had typical erythematous purpuric rashes in the lower extremities that were associated with warm weather and prolonged activity.
In the literature, authors have reported this phenomenon in adults, and in 1 case report, in a child. In 2016, Espitia et al performed a review of the literature and identified 99 adult patients, including 16 of their own patients, who had EIP, demonstrating that this is not an uncommon phenomenon in adults. Relapses in this cohort were common (78%), particularly when triggering conditions persisted. A histopathology revealed LCV in 95% of the cases. Kelly et al described 17 adult patients from Australia with these clinical features. The rash, which lasted 2 to 3 days, appeared either with golf (usually only after 18 holes of play) or hiking in warm weather. The mean age at onset was 56 years. Four biopsies in this cohort were consistent with LCV, revealing leukocytoclasis of neutrophils or lymphocytes, red blood cell extravasation, and endothelial cell swelling. Ramelet collected 23 patients from Switzerland with the same clinical features triggered by walking or hiking in warm weather. These patients had erythematous purpura (with occasional urticarial papules) appearing symmetrically on the lower leg. None of the children in our case series had accompanying urticaria. One of youngest published case reports is on a 19-year-old female patient who developed EIP after walking in flip-flops during the summer on a boardwalk. She developed red-purple papules around the outline of her flip-flop sandals. There is only 1 case report of suspected EIP in a child. This 11-year-old boy developed a petechial rash on his back and chest after sports activities. The location of his rash was atypical compared with the location in our case series as well as the typical location in the adult series.
In a report from the Netherlands, Prins et al had 58 patients participate in an 80 km march to study the prevalence of skin symptoms. Forty-one patients developed erythema and/or purpura. Eleven patients had biopsies performed. All 11 biopsies revealed LCV, with mild-to-severe leukocytoclasis as well as granulocytes and mononuclear cells invading the vessels. Three had marginal exocytosis of erythrocytes, and 2 had exocytosis of the infiltrate into the epidermis. The patients we described had a perivascular neutrophilic infiltrate with nuclear debris and erythrocyte extravasation, similar to that described in the adult literature.
It appears that the combination of activity and heat are the most significant contributing factors for EIP. Exercise in warm conditions may lead to muscular hyperthermia. In addition, the energy produced by muscular use can result in up to a 20-fold increase in muscular arterial flow. Poor augmentation to this high-venous load may cause increased capillary permeability, with leakage of blood cells into the surrounding tissues.
It has been suggested that EIP is a form of exercise-induced capillaritis. This condition has previously been classified as a benign cutaneous variant of LCV. Indeed, the language used to describe these lesions can be confusing. LCV is a histopathologic term to describe the microscopic changes. Cutaneous small-vessel vasculitis may be a more appropriate term to use, with the capillaries being the most frequently involved blood vessels. EIP may be best thought of as benign vasculopathy, not as a primary inflammatory vasculitis. The cutaneous manifestations are caused by exercise-induced venous hypertension and extravasation of red blood cells that, on biopsy, can reveal changes consistent with LCV. Neither our patients nor those in the adult literature were diagnosed with other disorders, and results of serological investigations were normal. Recognition of the typical presentation in children is paramount. EIP is a benign condition that is important to recognize to be able to provide reassurance to the patient and family and to avoid an unnecessary and costly evaluation. It should be noted that if patients have an atypical presentation of EIP, including unusual location of the rash, lack of described environmental and/or physical triggers, a prolonged duration, or accompanying systemic symptoms, consideration of an alternative diagnosis with an appropriate evaluation is prudent.